Strategizing from 7 cities across the globe
The Subconscious-Autonomic Nervous System Axis: A Novel Perspective on Neurodegenerative Disease Progression
Gaelle hankash


Introduction
The intricate relationship between the conscious and the unconscious, often associated with the complexity of human behavior, withholds a profound relationship with human health and may be the cause of many diseases. Although genetic predispositions, environmental factors, and mutations are the primary driving force explaining the prevalence of neurodegenerative diseases, individuals often overlook the importance of the cognitive and unconscious’ roles in their development. With its profound impact on cognition, the subconscious is a repertoire of beliefs, desires, and suppressed, learned behaviors operating beyond immediate introspection. As such, the psyche shapes physiological outcomes in an on overlooked manner in the framework of traditional biomedicine.
With the subconscious being at the foremost center of dilemmatic controversy between scientists, our research aims at unveiling the etiology behind the interplay of the mind and debilitating diseases. By influencing stress responses and immune functioning, the deeply embedded components of the mind that operate outside of conscious awareness may lead to chronic activation such as that of the hypothalamic-pituitary-adrenal (HPA) axis. Emotional trauma repressed psychological desires, or even Post Traumatic Stress Disorder (PTSD) can exacerbate neuronal damage. These psychological stressors manifest themselves as neuroinflammation, oxidative stress, and synaptic dysregulation which may exacerbate diseases’ progression, specifically in the context of neurodegenerative diseases such as Alzheimer’s disease (AD) and Parkinson’s (PD).
Our research endeavors to explore this intriguing interdisciplinary process by posing the central question of: to what extent do underlying cognitive biases contribute to the development and progression of neurodegenerative disorders? In doing so, our aim is to depict the interconnectedness of neuroscience and psychology, providing a clearer assessment of disease etiology and pathology.
By highlighting the interactions between the mind and the neural, this research’s goal is not only to comprehend the plethoric, discrepant forces influencing neuronal degeneration, but also simultaneously provide a domain for awareness, leading to earlier diagnosis and enabling early intervention. Our objective is to inspire novel therapeutic approaches and innovations to provide a more patient-centered care, acknowledging the pivotal importance of the cognitive, behavioral, and biological.
By first investigating the role of chronic stress in the pathophysiology of HPA and unveiling the autonomic nervous system’s responses, our research elucidated how subconscious patterns modulate nervous activity and promote the development of AD and PD. Through the lens of psychoneuroimmunology and neuroplasticity, we looked at how targeted interventions, such as cognitive behavioral therapy, mindfulness, and physical activity, can potentially modify subconscious drives and assist in delaying neurodegenerative diseases’ progression by promoting neural resistance.
Ultimately, our goal is to inspire a shift in the perception and management of neurodegenerative diseases by considering their deep connection to internal psychological factors. This perspective calls for a more holistic framework that accounts for cognitive, emotional, and biological dimensions of health, emphasizing the critical importance of early mental health care, stress management, and behavioral therapies in mitigating neurological decline.
Neurodegenerative Diseases: an Introduction to Pathophysiology
Alzheimer’s Disease
Expected to affect 13.8 million Americans by the year 2060, Alzheimer’s disease is the most common neurodegenerative disorder that is currently established by protein aggregates, specifically amyloid-beta plaques and neurofibrillary tangles composed of hyperphosphorylated tau protein, within the cerebral cortex and hippocampus (Karagas, 2025). These depositions disrupt synaptic communication, clinically manifesting itself with profound memory impairments, motor and executive dysfunctions, and language deficits.
Parkinson’s Disease
Characterized by a loss of dopaminergic neurons within the substantia nigra, a basal ganglia structure that plays a prominent role in motor control and movement, Parkinson’s disease is the second most common neurodegenerative disease after Alzheimer’s (Kouli, 2017). Affected patients show symptoms of tremor, rigidity, and bradykinesia, with postural instability appearing as the disease progresses. Pathologically, the accumulation of misfolded alpha-synuclein proteins into toxic clumps is an important indicator of disease progression. Acting as a waste clearance system, the glymphatic system that actively flushes out metabolic waste products including misfolded proteins becomes impaired in Parkinson’s, leading to cellular dysfunction within dopaminergic neurons (Massey, 2022).
The Subconscious
The subconscious mind, a subject of philosophical and psychological contention, refers to the part of mental life that operates beneath conscious awareness yet profoundly shapes thought, behavior, and perception. Psychoanalysts such as Freud conceptualized the subconscious as a repository of hidden desires and repressed memories, while modern theories frame it as a dynamic system that processes information automatically, without active intention (Arora et al., 2024). Scientifically, the subconscious encompasses implicit memory and automatic decision-making processes, essential cognitive functions that occur independently of conscious control. Hence, they are crucial in shaping habitual thoughts, orienting thinking patterns, and modifying emotional responses. Furthermore, other external factors such as chronic stress, social conditioning, trauma, and environmental exposure can mold subconscious processes over time, embedding cognitive biases that may go unrecognized by the individual. For instance, according to Das (2021), the subconscious is capable of independently initiating actions and processing information without conscious awareness. As such, this autonomy highlights the complexity of occurring mental processes that occur externally to consciousness.
The subconscious thus acts as a mental reservoir that gives one the ability to perform daily tasks, assess social cues, and analyze experiences that play a role in one’s understanding of the environment as well as their social circle, even if not consciously focusing on them. By comprehending the depth of emotions, the subconscious acts as a tool that allows one to reach for information kept in the back of their mind without the need to constantly access it. At a deeper level, it can be thought of as the mind’s operating system by directing automatic motor skills, such as the coordination of movements, and influencing implicit memory, by having past experiences shape current perceptions.
Novel, emerging research suggests that these biases alter neural circuits, influencing one’s susceptibility to neurodegenerative diseases or even aggravating the symptoms of patients.
Hypothalamus-Pituitary- Adrenal Axis and Neurodegeneration
From a scientific lens, the subconscious can be referred to as external processes occurring independently of conscious awareness while maintaining their ability to influence behavior and emotions, eventually affecting biological activities. Mediated by complex neural networks and neurotransmitter systems, the components of the subconscious play a complex role in the development of neurodegenerative diseases.
The amygdala is a central element of the limbic system and is involved in forming and processing emotional memories. Fear conditioning, the process by which a stimulus becomes correlated to a threat, occurs without conscious knowledge. Hence, if a person undergoes a negative, emotional experience, the amygdala is able to generalize the response to similar occurrences or even stimuli. With that, the learned fear response happens unconsciously without the entity recalling why they are afraid of the situation itself. As the amygdala projects directly to the paraventricular nucleus of the hypothalamus, the latter has an underlying function in the induction of stress responses through the hypothalamus-pituitary axis (HPA). During strain reactions, the hypothalamus produces the corticotropin-releasing hormone, activating the pituitary gland to produce adrenocorticotropic hormone and release it into the bloodstream, effectively stimulating the adrenal glands to release glucocorticoids such as cortisol during acute stressful environments. In the context of chronic stress and tension that may be the result of unconscious assimilation or Post Traumatic Stress Disorder (PTSD), the overactivation of the HPA and the increased level of cortisol in the blood may be detrimental and potentially lead to the development of Parkinson’s and Alzheimer’s diseases (P. & Vellapandian, 2024).
Although short-term cortisol level is adaptive and lowered by negative feedback mechanisms, the chronic elevation promotes “neuroinflammation, hippocampal atrophy, synaptic dysfunction,” causing atrophy in important regions involved in memory such as the hippocampus (P. & Vellapandian, 2024).
Regarding neuroinflammation, the exposure to high levels of the stress hormones exacerbates pro-inflammatory cytokines which damage neurons and lead to protein aggregation including beta-amyloid in Alzheimer’s and alpha-synuclein in Parkinson’s. Similarly, neuroinflammation is a pillar in the loss of neuronal plasticity which is involved in the formation and recalling of memories in the hippocampus, one of the most prominent symptoms of AD. To further elaborate, the heightened activation of cytokines and oxidative components contribute to dopaminergic neuron loss in the substantia nigra, the hallmark pathology of PD.
According to Sharan, “one of the main features of AD is the dysregulation of neuroendocrine functions particularly in the HPA axis” which appears to “be active in the early stages of AD pathology, prior to the manifestation of behavioral symptoms and cognitive impairment” (2024).
Thus, traumatic experiences, especially during childhood or early in life, may program the brain to remain in a constant, hypervigilant state of stress, even long after being conscious about the situation and suppressing it in the subconscious or unconscious. Being in a perpetual state of fight or flight leads to the activation of elevated glucocorticoids levels which may potentially lead to the emergence of the most common neurodegenerative diseases.
The Autonomic Nervous System and Neurodegenerative Disorders
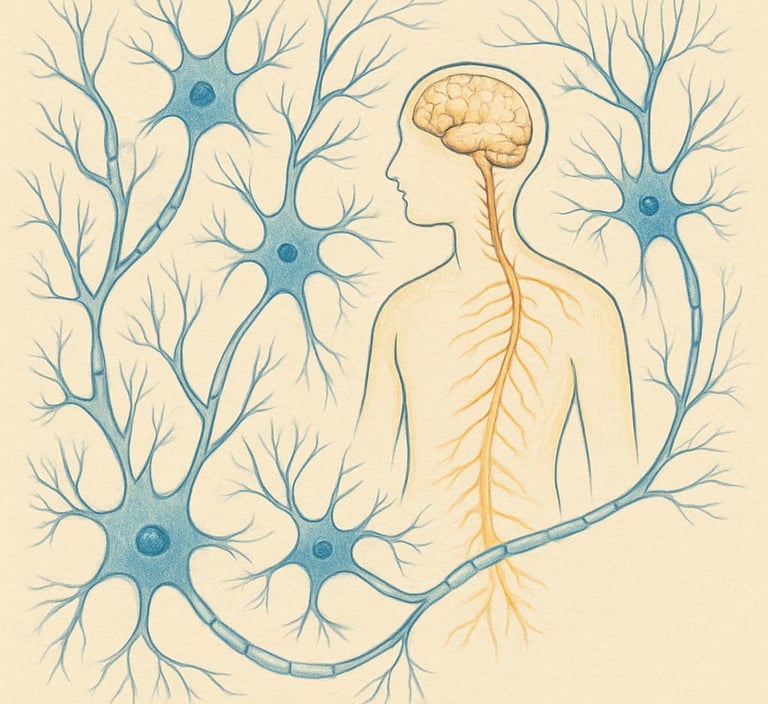
As a major division of the peripheral nervous system, the Autonomic Nervous System (ANS) is a vital unconscious control system that organizes the body’s internal environment, orchestrates physiological responses to external stimuli, and ensures adaptability to maintain homeostasis without necessitating conscious effort. Constituting of the sympathetic and parasympathetic branches, the ANS innervates all internal organs, glands, and smooth muscles. Through its control, it regulates essential involuntary physiological processes such as heart rate, blood pressure, respiration, digestion, body temperature, and pupillary response.
Although the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS) exert antagonist effects on the human body, they are necessary in the maintenance of internal homeostasis (Wulf & Tom, 2021). The SNS is responsible for the fight or flight response which is activated during perceived threats or sudden stressful situations. Upon stimulation, it triggers a cascade of physiological changes by commencing with the release of acetylcholine by the preganglionic neuron that emerges from the thoracolumbar region of the spinal cord and ends with the release of norepinephrine from postganglionic neurons and epinephrine/norepinephrine from the adrenal medulla into the bloodstream (Wulf & Tom, 2021). This efficiently contributes to increased heart rate and contractions, dilated airways and blood vessels to skeletal muscles, constricted blood vessels to non-essential organs, enhanced oxygen uptake, and even the mobilization of stored energy reserves, preparing the body for quick responses.
On the other hand, the parasympathetic nervous system (PNS) is more involved in resting, digesting, and repairing. Its primary role is to conserve energy and promote digestive or anabolic processes that are necessary for maintenance and repair, completely opposing the role of the SNS. According to Wulf and Tom (2021), the PNS releases acetylcholine at both preganglionic and postganglionic synapses. At first, it binds to nicotinic receptors on the postganglionic neuron to excite it; however, when emerging from postganglionic-effector synapse, the neurotransmitter binds to muscarinic receptors on effector cells to produce the PNS effects, determining the correct physiological response that should occur.
Heavily influenced by both internal and external stimuli, the autonomic nervous system is highly susceptible to the influence of subconscious biases that are shaped by prior experience and trauma. By having the subconscious at the forefront of directing one’s activity, suppressed stressful situations may turn into chronic ones, leading to the overactivation of the SNS and inhibition of PNS. Hence, the subconscious impacts the autonomic nervous system which may lead to the development of neurodegenerative diseases.
According to Giunta et al. (2023), the overactivation of the sympathetic nervous system promotes pro-inflammatory conditions that exacerbate with the diminished activity of the PNS. This causes anti-inflammatory effects mediated by the cholinergic anti-inflammatory pathway (CAP), a neural mechanism that bridges the nervous and immune systems, playing a vital role in controlling and reducing systemic inflammation. Thus, by having CAP weakened, chronic inflammation persists and exacerbates. Unchecked neuroinflammation and dysregulation contribute to the progression of Alzheimer’s and Parkinson’s. Onyango et al. (2021) reveal that neuroinflammation plays a central role in its etiopathogenesis of Alzheimer’s disease owing to its capacity to “exacerbate Aβ and τ pathologies due to high microglia activation”, indicating that inflammation leads to disease progression.
Therefore, the dysregulation of the balance between SNS and PNS, often induced by subconscious biases toward negativity, hypervigilance, and fear, can diminish vagal tone, thereby reducing the protective parasympathetic response. This imbalance has been implicated in the early pathophysiological changes of neurodegenerative diseases such as Parkinson’s and Alzheimer’s. For example, in Parkinson’s disease (PD), dysautonomia often precedes motor symptoms and includes gastrointestinal dysfunction and orthostatic hypotension, both linked to alpha-synuclein pathology in autonomic ganglia (Olivieri et al., 2024). Similarly, in Alzheimer’s disease (AD), impaired cholinergic transmission is a core pathological feature, and parasympathetic dysfunction may accelerate amyloid-beta deposition and tau hyperphosphorylation through impaired clearance mechanisms.
Further research has looked into the impaired activity of the HPA axis as a result of neuroinflammation which is enhanced by stress induced coping mechanisms caused by the overexcitability of the ANS and inhibition of the PNS. It is also necessary to note that neurotransmitters modulated by the ANS, such as dopamine and acetylcholine, which play essential roles in maintaining neuronal integrity and synaptic plasticity, become more vulnerable to oxidative stressful environments. In fact, dopaminergic neurons in the substantia nigra pars compacta are more prone to degeneration, which may be exacerbated by prolonged sympathetic overactivity and associated mitochondrial dysfunction caused by HPA axis dysregulation. Hence, subconscious biases that predispose an individual toward chronic psychological stress may initiate or accelerate neurodegenerative cascades via persistent dysregulation of the ANS.
Treatment, prevention, and intervention
Cognitive Behavioral Therapy
With the aim of identifying and altering the maladaptive thoughts and suppressed emotions of an individual, cognitive behavioral therapy is a novel psychotherapy technique used for the purpose of helping individuals recognize unhealthy ideas. Although this method operates at a conscious level, its effects are profound enough to impact subconscious processes that create chronic negative thought patterns. For instance, CBT first aids with the recognition and reconstruction of autonomic negative thoughts (ANTs) which are unquestioned thoughts that automatically and involuntarily arise from the subconscious. The latter might include statements similar to “I cannot cope”, “I am not worthy enough”, “Everything is always going wrong”. Although one can distinguish the positive stage of life they are in, they might always have these unbearable thoughts without knowing why. As a result of accumulated, repressed situations that someone often ignores and chooses not to think about, one has the tendency to dispose these instances into the subconscious and only relive these moments when resurfaced due to conscious recalling. CBT teaches individuals to identify these unmotivating and degrading thoughts, challenge their validity, and modify or even replace them with more realistic cognition. By doing so, CBT indirectly reduces the frequency, intensity, and prevalence of stress responses, leading to reduced chronic HPA axis activation, eventually aiding in less severe symptoms of neuronal degeneration. In fact, according to Wu et al. “22 studies incorporating 1,053 PD patients treated with CBT were evaluated, revealing improved cognition, QoL, anxiety, and depression following such [CBT] treatment” (2024). Prior to that, MRI scans have depicted the decreased activity in the limbic areas, involved in fear and emotional processing, in patients suffering from anxiety disorders and increased activity in the prefrontal cortical areas that are responsible for executive functions and reasoning. Effectively, with tactics promoting stress management and mindfulness, CBT encourages cognitive engagement strengthening neuroplasticity, the brain’s ability to create new connections. As such, CBT significantly enhances regulatory recovery, allowing a more modulated HPA axis response and lowered cortisol secretion, aiding in combatting AD and PD symptoms.
Exercise and Neuroplasticity:
As a form of escape and strong coping mechanism, physical activity has proven to be an effective method to reduce stress and improve mental health. By triggering the surge of endorphins, serotonin, and dopamine, exercise provides a sense of well-being which positively impacts the subconscious emotional states.
This neurochemical surge provides an immediate, "subconscious" mood boost and can act as a powerful antidepressant. Thus, this physiological effect, initially felt consciously, becomes implicitly associated with relief and well-being. With regular, controlled physical stress during exercise, both brain and body learn to better handle physiological arousal or stressful situations. As such, the autonomic nervous system regulates itself to activate and deactivate distinctively more efficiently rather than having an overactive fight or flight response. This improved regulation helps exercise contribute to enhanced neuroplasticity by promoting a well-balanced subconscious state.
Research clearly establishes a deep interconnection between exercise and neuroplasticity. For example, with the aim of depicting improved neuroplasticity in people with Parkinson’s as a result of exercise, Garavito et al. elucidated the extent to which physical activity significantly increases levels of Brain-Derived Neurotrophic Factor (BDNF), Vascular Endothelial Growth Factor (VEGF), and Insulin-like Growth Factor 1 (IGF-1), which are crucial for neurogenesis, particularly in the hippocampus, and in the formation of new synapses along with increased plasticity (2025).
Aside from its contribution to neurotrophic factor, exercise also ameliorates blood flow to the brain. This enhances oxygen and nutrient delivery and supports the health of the cerebrovascular system, allowing the glymphatic system to efficiently clear toxic buildup – a key significant contributor in the pathology of PD. Moreover, physical activity reduces neuroinflammation, activated by microglia and astrocytes which exacerbate the development of PD, by reducing the production of pro-inflammatory cytokines.
According to Seo et al.’s study (2019), exercising considerably inhibited neuroinflammation by lowering the expression of “pro-inflammatory factors and increasing the expression of anti-inflammatory factors”. This statement can be further supported by Kim et al.’s study (2017) in which they demonstrated how 20 weeks of treadmill running improved neuroinflammation and reduced neuronal apoptosis. Additionally, Tuon et al. (2012) revealed that exercise regulated α-synuclein activity, BDNF, and sarcoplasmic reticulum Ca2+ ATPase levels in PD animal models. Exercise was also shown to regulate GDNF gene expression, which is crucial for the survival of dopaminergic neurons. Therefore, these results demonstrate how exercise, by indirectly inhibiting the factors that enhance the development of neurodegenerative diseases, might be one of the most promising therapeutic approaches in delaying their progression.
Meditation and Neuroplasticity:
Meditation, including Mindful Meditation Training (MMT), offers a profound, intricate pathway to ameliorate one’s relationship with the deeply embedded patterns of the subconscious by bringing automatic thoughts and emotions to awareness. It efficiently trains the mind to interact with ANTS that impact mood and cognition. By aiding the brain to shift from the sympathetic nervous system, correlated with fight or flight responses, to the parasympathetic one, linked to resting activities, meditation implicitly reprograms emotional responses and perceived threats that emerge from subconscious thoughts. Aside from assisting with cultivating non-judgmental awareness, meditation consistently enhances neuroplasticity which in turn slows the development of neurodegenerative diseases.
A plethora of studies have revealed that regular MMTs can reduce stress and anxiety while strengthening neuronal connections and improving neuroplasticity. For example, Álvarez et al. (2023) noticed increased “activity in the superior frontal gyrus, posterior cingulate cortex, and right hippocampus during the alerting condition of the ANT after the MMT; decreased stress and trait anxiety were significantly correlated with the activation in the right hippocampus”. Through DTI imaging, this study suggested increased fractional anisotropy in the right uncinate fasciculus of the MMT group, suggesting improved white matter microstructure between the right hippocampus and frontal brain regions which are indicative of neuroplastic adaptations. Moreover, Leung et al. (2018) revealed decreased activity in the amygdala of awareness-based compassion meditation’s participants. Prior to that, other studies elucidated a decrease in size of amygdala (Gotink et al., 2019). Hence, while assisting with neuroplastic rewiring, meditation encourages a shift from overactive stress responses to emotional regulation. With that, less chronic neuroinflammation and dysregulation in the HPA axis persevere, delaying the neuronal damage associated to Alzheimer’s and Parkinson’s. To add, meditative activities foster ameliorated sleep quality which indirectly ameliorates the efficiency of the glymphatic system that is most active during sleep.
Future research
To unravel the complex interrelation between the subconscious and the progression of neurodegenerative diseases, future research should delve deeper into quantifying the precise mechanisms by which subconscious processes impact dysregulation and contribute to neurodegenerative pathologies.
One suggestion is to quantify the ways by which the subconscious influences the autonomic nervous system’s dysregulation through the integration of physiological monitoring and neuroimaging. Physiologically, researchers should monitor heart rate variability to assess vagal tone, skin conductance responses indicating sympathetic arousal, and pupillometry, which are all indicators of subconscious emotional processing’s responses mediated by the ANS. Advanced neuroimaging techniques should be utilized in parallel to reveal real-time changes in brain regions associated with subconscious stimulation. For instance, functional magnetic resonance (fMRI) can demonstrate the amygdala’s activity as a result of threat perception and its impact on the ANS or even the HPA axis. Zhou et al. (2021) show the importance of using Visually Induced Fear Signature (VIFS), an fMRI-based model capable of predicting individuals' self-reported fear levels in response to visual stimuli, to assess subcortical systems activation. Hence, while subjecting participants to stimuli that trigger threat activation correlated to the subconscious, researchers will be able to mediate defensive responses by observing interactions between the amygdala and the hypothalamus-pituitary-adrenal axis. Additionally, Positron Emission Tomography (PET) scans may be employed to track the accumulation of neurodegenerative, toxic biomarkers including beta-amyloid plaques and alpha-synuclein aggregates as well as inflammatory markers. Through these techniques, scientists can understand and unveil the specific patterns by which subconsciously driven ANS deregulatory responses may accelerate neurodegenerative diseases’ pathology and aggravate their symptoms’ manifestations, offering necessary information for early detection and intervention as well as holistic treatment options.
Another suggestion is to develop and test novel therapeutic approaches to modify maladaptive subconscious patterns. For example, future research can focus on implicit bias training and mindfulness strategies that help reshape automatic emotional responses a result of subconscious biases. Consequently, researchers might even assess the efficiency of PTSD therapies in resolving subconscious, emotional patterns that lead to chronic stress and ANS dysregulation. By modifying existing approaches, studies will be able to assess whether these early interventions delay or even prevent the symptoms of AD and PD. Therefore, by addressing the root of the subconscious’ mishaps, this interdisciplinary approach promises personalized treatment strategies.
Conclusion
In conclusion, this paper unraveled the profound, often biomedically disregarded, interplay between the subconscious mind and the progression of neurodegenerative diseases such as Alzheimer’s and Parkinson’s. We have explored the role of the autonomic nervous system, that operates independently of conscious awareness, acts as the major mediator between the two studied factors, and impacts on the exacerbation of symptoms. As subconscious biases are molded by past experiences, they effectively set out to instigate chronic activation of the sympathetic nervous system, which in turn inhibits the activity of the parasympathetic one. As such, CAP leads to neuroinflammation and HPA dysfunction. With hypothalamus-pituitary-adrenal axis dysregulation, increased cortisol levels are accompanied, further promoting the release of pro-inflammatory cytokines and exacerbating neuroinflammation. This eventually contributes to the accumulation of toxic protein aggregates such as beta-amyloid, tau, and alpha-synuclein, driving neuronal degradation.
To address these pathological processes, this research underscores the necessity of adopting holistic and integrative treatment strategies. It emphasized the role of neuroplasticity, which determines how the brain is able to rewire itself in preventing disease progression, as a protective mechanism against neuronal degeneration. Interventions such as cognitive behavioral therapy, physical exercise, and meditation may be used as non-pharmaceutical approaches to harness neuroplasticity and modify maladaptive subconscious patterns. Through the application of neuroimaging and personalized therapeutic models, it may be possible to monitor disease progression more precisely and tailor interventions to individual cognitive and physiological profiles.
Finally, this paper advocates for the importance of integrating early mental health interventions within a comprehensive framework for the prevention and management of neurodegenerative diseases. It aims to encourage future research to explore the use of early psychological care and proactive stress management as tools to assess disease pathology and monitor symptom manifestation through neuroimaging, thereby advancing the development of personalized therapeutic strategies.

Download the full document
References
Leung, M. K., Lau, W. K. W., Chan, C. C. H., Wong, S. S. Y., Fung, A. L. C., & Lee, T. M. C. (2017). Meditation-induced neuroplastic changes in amygdala activity during negative affective processing. Social Neuroscience, 13(3), 277–288. https://doi.org/10.1080/17470919.2017.1311939
Guidotti, R., Del Gratta, C., Perrucci, M. G., Romani, G. L., & Raffone, A. (2021). Neuroplasticity within and between functional brain networks in mental training based on long-term meditation. Brain Sciences, 11(8), 1086. https://doi.org/10.3390/brainsci11081086
Mora Álvarez, M. G., Hölzel, B. K., Bremer, B., Wilhelm, M., Hell, E., Tavacioglu, E. E., Koch, K., & Torske, A. (2023). Effects of web-based mindfulness training on psychological outcomes, attention, and neuroplasticity. Scientific Reports, 13(1). https://doi.org/10.1038/s41598-023-48706-0
Seo, D.-Y., Heo, J.-W., Ko, J. R., & Kwak, H.-B. (2019). Exercise and neuroinflammation in health and disease. International Neurourology Journal, 23(Suppl 2). https://doi.org/10.5213/inj.1938214.107
Kim, D., Cho, J., & Kang, H. (2019). Protective effect of exercise training against the progression of alzheimer’s disease in 3xTg-Ad Mice. Behavioural Brain Research, 374, 112105. https://doi.org/10.1016/j.bbr.2019.112105
Johansson, H., Hagströmer, M., Grooten, W. J., & Franzén, E. (2020). Exercise-induced neuroplasticity in parkinson’s disease: A metasynthesis of the literature. Neural Plasticity, 2020, 1–15. https://doi.org/10.1155/2020/8961493
Wu, X., Shi, M., Lian, Y., & Zhang, H. (2024). Cognitive behavioral therapy approaches to the improvement of mental health in parkinson’s disease patients: A systematic review and meta-analysis. BMC Neurology, 24(1). https://doi.org/10.1186/s12883-024-03859-x
Romero Garavito, A., Díaz Martínez, V., Juárez Cortés, E., Negrete Díaz, J. V., & Montilla Rodríguez, L. M. (2025). Impact of physical exercise on the regulation of brain-derived neurotrophic factor in people with Neurodegenerative Diseases. Frontiers in Neurology, 15. https://doi.org/10.3389/fneur.2024.1505879
Wulf, M. J., & Tom, V. J. (2023). Consequences of spinal cord injury on the sympathetic nervous system. Frontiers in Cellular Neuroscience, 17. https://doi.org/10.3389/fncel.2023.999253
Olivieri, F., Biscetti, L., Pimpini, L., Pelliccioni, G., Sabbatinelli, J., & Giunta, S. (2024). Heart rate variability and autonomic nervous system imbalance: Potential biomarkers and detectable hallmarks of aging and inflammaging. Ageing Research Reviews, 101, 102521. https://doi.org/10.1016/j.arr.2024.102521
Onyango, I. G., Jauregui, G. V., Čarná, M., Bennett, J. P., & Stokin, G. B. (2021). Neuroinflammation in alzheimer’s disease. Biomedicines, 9(5), 524. https://doi.org/10.3390/biomedicines9050524
Arora, Ms. J. (2024). Exploring consciousness and the subconscious mind: A comparative study of the panchkosha theory and freud’s unconscious. Revista Electronica De Veterinaria, 1244–1248. https://doi.org/10.69980/redvet.v25i2.1747
Das, K. K. (2021). Consciousness and Its Relation with Subconscious Mind: The Mystery Probed. https://doi.org/10.31234/osf.io/wu8m7
Kouli, A., Torsney, K. M., & Kuan, W.-L. (n.d.). Parkinson’s Disease: Etiology, Neuropathology, and Pathogenesis. essay.
Karagas, N., Young, J. E., Blue, E. E., & Jayadev, S. (2025). The spectrum of genetic risk in alzheimer disease. Neurology Genetics, 11(1). https://doi.org/10.1212/nxg.0000000000200224
Nikolenko, V. N., Oganesyan, M. V., Rizaeva, N. A., Kudryashova, V. A., Nikitina, A. T., Pavliv, M. P., Shchedrina, M. A., Giller, D. B., Bulygin, K. V., & Sinelnikov, M. Y. (2020). Amygdala: Neuroanatomical and morphophysiological features in terms of neurological and neurodegenerative diseases. Brain Sciences, 10(8), 502. https://doi.org/10.3390/brainsci10080502
P, S., & Vellapandian, C. (2024). Hypothalamic-pituitary-adrenal (HPA) axis: Unveiling the potential mechanisms involved in stress-induced alzheimer’s disease and depression. Cureus. https://doi.org/10.7759/cureus.67595
Zhou, F., Zhao, W., Qi, Z., Geng, Y., Yao, S., Kendrick, K. M., Wager, T. D., & Becker, B. (2021). A distributed fmri-based signature for the subjective experience of fear. Nature Communications, 12(1). https://doi.org/10.1038/s41467-021-26977-3
