Strategizing from 7 cities across the globe
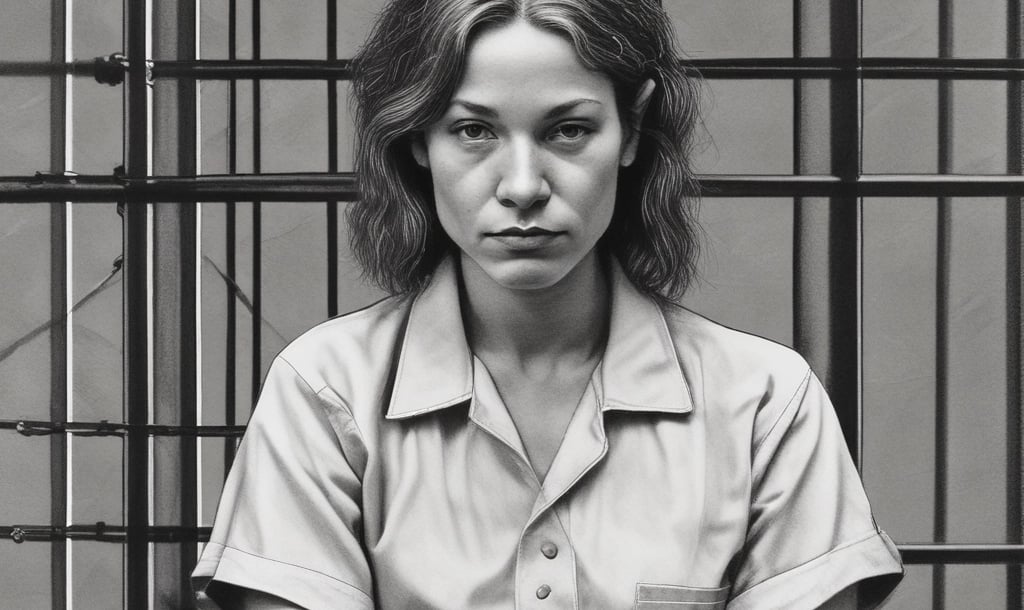
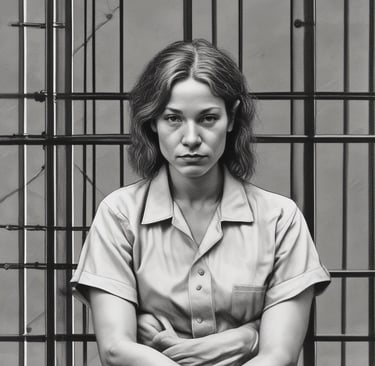
Mental Health Behind Bars: Addressing Challenges Faced by Incarcerated Women
One critical yet overlooked aspect of public health includes women’s health in prison, especially given the significant increase in the global prison population. As of October 2021, more than 10.77 million people were held in penal institutions, but estimates allude that the true number reaches 11.5 million. This is due to the uncounted prisoners held under unrecognized authorities or pre-trial detainees
MENTAL HEALTHHEALTHCARETRAUMALAWCIVIL SOCIETYDEMOCRACY
Jennifer El Asmar
12/8/20248 min read
Introduction
One critical yet overlooked aspect of public health includes women’s health in prison, especially given the significant increase in the global prison population. As of October 2021, more than 10.77 million people were held in penal institutions, but estimates allude that the true number reaches 11.5 million. This is due to the uncounted prisoners held under unrecognized authorities or pre-trial detainees (Fair, 2021). Out of these, 740,000 are women and girls, reflecting a 60% increase in number since the year 2000 in comparison to a 22% rise in males at the same time. The United States alone accounts for approximately 211,375 sentenced female prisoners, thereby contributing to the highest incarceration rate globally of 629 prisoners per 100,000 population (Fair, 2022). These findings, drawn from the Institution for Crime & Justice Policy Research (ICPR), highlight the urgent need to address the mental health challenges these women face in prison.
As a punishment for illegal activity, prisons serve as a direct means to detain individuals accused of an unlawful act. Coyle (2005) states that the scope of punishment includes sentencing criminals, safeguarding the community from offenders, deterring possible offenders, and reducing recidivism. Considering the burden prisons bring on taxpayers’ shoulders, with each UK prisoner’s cost even reaching £35,000 annually, the most prioritized concern is how realistic and achievable these goals are. Although such goals and resources provide a sound basis for the system, the legitimacy of imprisonment as a punishment is always under scrutiny. It is observed that re-offending rates are alarmingly high which suggests that some purposes of imprisonment such as deterrence or rehabilitation do not achieve desired results. For instance, it was reported by the Social Exclusion Unit (2009) that within two years of being released, approximately 60% of ex-prisoners commit another crime and go back to jail, and 20% of crimes that take place overall are contributed to by ex-prisoners. Furthermore, imprisonment has significant unintended consequences, including increasing drug misuse, declining physical and mental health, and surging rates of prisoner suicide (Dye, 2010). These impacts appear to be particularly pronounced in women who are already vulnerable and have a variety of mental health issues or are suffering from the stressful consequences of prison. This research examines these concerns through the lens of the Importation and Deprivation Models, contrasting the mental health outcomes of women with and without preexisting mental health conditions. It also assesses the quality of mental health treatment in prisons and recommends some public health measures to address these critical issues.
The Importation and Deprivation Models
The importation model posits that maladaptive behaviors, such as poor mental health, are brought into the prison setting by individuals themselves. Proponents of this model argue that mental health issues are contributors to criminal behavior, leading to arrest and incarceration (Edwards & Potter, 2004). This suggests that pre-existing afflictions and characteristics of prisoners mostly explain the high prevalence of mental illness within prison populations, hence the name “imported”.
On the other hand, the deprivation model relates the development of mental illness to the harsh conditions and "pains of imprisonment" experienced in the prison environment. A major criticism of this model is its failure to explain why some individuals develop mental health problems while others do not (Dye, 2010). If deprivation alone leads to maladaptation, then all prisoners are expected to experience mental health issues. However, numerous studies conducted by Fazel and Danesh (2002) show that this is not the case. Similarly, the importation model also has its limitations, as it tends to downplay and overlook the effects of deprivation (Dye, 2010). It implies that prisoners are not influenced by the prison environment that they’re in, which contradicts existing evidence.
Research on prison suicides suggests that a combination model offers a more comprehensive explanation of the phenomenon (Blaauw, 2001). In this view, suicide, which can be seen as a type of maladaptation, can arise from the accumulation of pre-existing vulnerabilities and the stressors related to deprivation experienced during incarceration. A similar look and rationale can be applied to mental illness, where the "pains of imprisonment" exacerbate existing mental health conditions and traits. This perspective helps clarify why some individuals are more vulnerable to mental illness while in prison than others and it patches up the empty spaces left by the missing points of each model individually.
How Prison Affects Women with Pre-Existing Mental Health Issues (Importation)
Many women who enter prison often suffer from mental health issues pre-incarceration making them more vulnerable in prison environments. The Office for National Statistics (ONS) conducted a study on psychiatric conditions among prisoners in England and Wales in 2024 and found that 40% of incarcerated women had sought help or treatment for mental or emotional issues in the year preceding their imprisonment. Similarly, Caulfield's 2016 study, which involved 43 women in prison, revealed that 27 of them reported experiencing mental health and emotional challenges prior to their current sentence, whether formally diagnosed or not. These ranged from PTSD, depression, and anxiety, and some were accompanied by self-harm and suicidal thoughts. Among these, depression stood out as the most common issue, reported by 23 of the 27 participants. The same study showed that women placed in high-security prisons often suffer the most mentally. These go back to factors that include childhood violence, weaknesses, or lack of social support, which makes them more prone to be involved in violent crimes. Even though the relationship between women’s background and their mental health in association with their criminal history is a complex one, little to no attention has been drawn to it in prison, which is evident by the high rates of undiagnosed, misdiagnosed, or ill-treated women (Caufield, 2016).
Mental health issues among women are not reduced when they enter prison. This is especially true for women struggling with substance abuse, as they often experience an increase in mental health problems during the detoxification process. As their bodies clear out the drugs, the “numbing” effect they relied on is lifted off, causing all the unresolved issues they were trying to escape to resurface, often overwhelming them. It is important to add that a significant percentage of incarcerated women are mothers, and that mother-child separation exacerbated the depression for diagnosed women. The latter report feelings of guilt, shame, disparity, and frustration at having “abandoned” their children. Other women experienced insomnia and reported that it was because of their time away from their children, although they explained that they were previously diagnosed with paranoia and severe anxiety. Others reported that they were placed on a suicide watch because of their previous suicide attempts. Less severe cases represent tension headaches experienced outside the prison and that was reported to increase in severity inside. (Caufield, 2016). These findings align with the importation theory, which suggests that the challenges women face in prison often stem from pre-existing issues they bring with them into the prison environment.
How Prison Affects Women with No History of Mental Health Issues (Deprivation)
Incarceration often leads to the development of mental health issues in women who had no previous diagnosis. From a trauma deprivation (or exacerbation) model perspective, prison can have severe detrimental effects on women’s mental health. Indeed, Kenning et al. (2010) showed that traumas experienced in prison, such as relocation depression, verbal and emotional abuse from prison staff, and the invasion of privacy contribute to mental illness problems among incarcerated women.
Many women reported that shortly after being arrested, they entered depressive episodes and were prescribed anti-depressant medication. Others shared that they developed eating disorders as they struggled to cope with their new environment. One woman in the Kenning et al. study expressed how difficult it was to accept that she had transitioned from living a 'normal' life to being behind bars, separated from her family. Another woman described how her poor mental health affected her physical well-being, causing painful headaches, especially as she was in denial about feeling anxious or depressed.
In numerous cases, women in prison felt disempowered and often resorted to self-harm as a means of asserting some control over their lives. They reported that the urge to self-harm was uncontrollable and impulsive, stemming from feelings of anger, frustration, and disappointment. One woman from Kenning et al.'s report described her experience with self-harm:
I’ll just sit there thinking about my past, you know, how I ended up in prison, how I’ve let my kids down, and then I just get really, really worked up, and I have to see blood to relieve my pain. (P8:437)
Furthermore, many women faced emotional abuse from prison staff and officers, who often reacted to self-harming behavior by labeling it as a plea for attention or a manipulation tactic to get benefits. This perspective made these women seem less deserving of care and support within the prison system (Kenning et al., 2010).
The loss of privacy, particularly by nursing staff, has been a significant source of stress for incarcerated women and negatively impacts their mental health. Nurses often accompany them to medical appointments, acting as their guardians, but frequently interfere by interpreting the women's symptoms and conditions instead of respecting their dignity and confidentiality (Plugge et al., 2008). Furthermore, women report feeling looked down upon by officers, which leads to subpar healthcare due to these prejudices. Regarding emotional wellness after therapy sessions, women have expressed that the information provided about their health is overly simplistic and that there is insufficient communication regarding the serious nature of their conditions (Ahmed et al., 2016). These experiences illustrate how the prison environment not only fails to protect the mental health of women without prior conditions but actively contributes to their psychological deterioration, fostering cycles of trauma and neglect.
Conclusion:
Many women enter prison with existing mental health issues, while others develop such problems due to the tough challenges of incarceration. Irrespective of both scenarios, this paper highlighted systemic failures in addressing their needs, revealing how prisons often exacerbate vulnerabilities rather than providing the support necessary for recovery. Instead of achieving their so-called role in rehabilitation, prisons strip women of their agency and neglect their mental health, leaving them ill-equipped to stand back on their feet upon their release. Bartlett and Hollins (2018) emphasize that women’s criminal behavior must be understood within the context of trauma, and they stress the importance of prisons serving as environments where quality mental health care is prioritized.
Recovery in prison involves finding new meaning and purpose for prisoners’ lives. Achieving this requires proper mental health care, but this is unattainable without systemic reforms. Prison staff hold a crucial role in addressing this issue by advocating for mental health interventions and abiding by systems that respect confidentiality and dignity. In addition to this, educating staff on mental health helps for a deeper understanding of the problems faced by incarcerated women, promoting a more compassionate approach to care. Another conclusion reached from this paper is that marginalized women in prison who are already at risk for poorer mental health outcomes face further marginalization within the literature community with insufficient studies into their specific needs. Without targeted reforms and programs, prisons will continue to fall short of their rehabilitative purpose, leading to cycles of recidivism, and failing to prepare women for life beyond its walls.
References:
Ahmed, R., Angel, C., Martel, R., Pyne, D., & Keenan, L. (2016). Access to healthcare services during incarceration among female inmates. International Journal of Prisoner Health, 12(4), 204–215. https://doi.org/10.1108/IJPH-04-2016-0009
Bartlett, A., & Hollins, S. (2018). Challenges and mental health needs of women in prison. The British Journal of Psychiatry, 212(3), 134–136. https://doi.org/10.1192/bjp.2017.42
Blaauw, E., Kerkhof, A., Winkel, F., & Sheridan, L. (2001). Identifying Suicide Risk in Penal Institutions in the Netherlands. The British Journal of Forensic Practice, 3(4), 22–28. https://doi.org/10.1108/14636646200100024
Caulfield, L. S., & Twort, H. (2016). Implementing change: Staff experiences of changes to prison mental healthcare in England and Wales. International Journal of Prisoner Health, 8(1), 7–15. https://doi.org/10.1108/17449201211268246
Coyle, A. (2005). Understanding prisons: Key issues in policy and practice. Open University Press.
Dye, M. H. (2010). Deprivation, importation, and prison suicide: Combined effects of institutional conditions and inmate composition. Journal of Criminal Justice, 38(4), 796–806. https://doi.org/10.1016/j.jcrimjus.2010.05.007
Edwards, W. T., & Potter, R. H. (2004). Psychological Distress, Prisoner Characteristics, and System Experience in a Prison Population. Journal of Correctional Health Care, 10(2), 129–149. https://doi.org/10.1177/107834580301000202
Fair, H., & Walmsley, R. (2021). World Prison Population List- thirteenth edition.
Fair, H., & Walmsley, R. (2022). Women and girls in penal institutions, including pre-trial detainees/remand prisoners.
Fazel, S., & Danesh, J. (2002). Serious mental disorder in 23 000 prisoners: A systematic review of 62 surveys. The Lancet, 359(9306), 545–550. https://doi.org/10.1016/S0140-6736(02)07740-1
Kenning, C., Cooper, J., Short, V., Shaw, J., Abel, K., & Chew‐Graham, C. (2010). Prison staff and women prisoner’s views on self‐harm; their implications for service delivery and development: A qualitative study. Criminal Behaviour and Mental Health, 20(4), 274–284. https://doi.org/10.1002/cbm.777
Office for National Statistics. (n.d.). User guide to crime statistics for England and Wales: March 2024.
Plugge, E., Douglas, N., & Fitzpatrick, R. (2008). Patients, prisoners, or people? Women prisoners’ experiences of primary care in prison: a qualitative study. British Journal of General Practice, 58(554), e1–e8. https://doi.org/10.3399/bjgp08X330771
Social Exclusion Task Force (2009). Short study on women offenders. London: Social Exclusion Task Force.
